Weight loss is one of the common symptoms of lymphoma and one of the most common side effects of lymphoma treatments, especially chemotherapy.
Weight loss was a real problem for me, especially in the first couple of months of my diagnosis. At one point, I lost 12kg, nearly 20% of my body weight, and despite eating 4,000 calories a day I wasn’t putting on weight. It was very worrying and depressing to see my physical appearance change so rapidly and to feel as though my body was wasting away.
Thankfully, my weight loss lessened as the treatment progressed and I was even able to slowly put some weight back on while having chemotherapy.
Causes of lymphoma weight loss
Lymphoma itself
Lymphoma itself causes weight loss1Macmillian | Signs and symptoms of lymphoma. This is due to the cancerous cells using up energy at the same time as your body is using energy trying to fight them2Lymphoma Action | Symptoms of lymphoma. Before my diagnosis, some of my friends commented that I appeared to be losing a lot of weight.
Some treatments against high-grade and bulky lymphoma work very quickly, within days in my case. Once I started chemotherapy and steroids, I began to lose a lot of weight. This was mostly due to the huge volume of lymphoma that I had breaking down. I was prescribed Allopurinol, to help my body cope with the byproducts of this rapid breakdown. At this stage, the weight loss was at its most severe.
Taste changes
Within a couple of days of starting chemo, my ability to taste food and drink changed. I had a constant unpleasant taste in my mouth and food and drink didn’t taste the same. I quickly got used to this and through experimentation learned which foods and drinks tasted better (well, less bad) when my taste was affected.
Nausea, vomiting and diarrhoea
Chemotherapy often causes nausea, vomiting and diarrhoea. I had all these at various points in the treatment (including plenty of embarrassing incidents of throwing up in the hospital car park and on the high street). They really made maintaining my weight a challenge as I lost my appetite and just didn’t feel like eating. The doctors prescribed various anti-emetics, which did help.
Persistent hiccups were also an unexpected annoyance of my chemo!
Mucositis
During the third cycle of DA-EPOCH-R chemotherapy, I began to have problems with mucositis (mouth sores and saliva changes). This usually happened in the second week of the cycle and got progressively worse with each cycle (possibly because the dose was being increased). The mucositis would usually only last 5-7 days, so I was able to plan it to some degree.
I followed all the guidance on mouth hygiene religiously, but I wasn’t able to stop the mucositis. During the fifth cycle, I had to be hospitalised as I couldn’t eat or talk, and my CRP markers were elevated due to all of the mouth and throat sores. This was really one of the most horrible times of my whole treatment. I was prescribed lidocaine, which did help, and it enabled me to eat a bit of porridge and soup each day. Ice cream and ice lollies helped me get a few extra calories and numb the pain a little bit throughout the day.
Hospital food
NHS hospital food is truly terrible! I had over 12 stays in the hospital and each time my weight went down. Being on the haematology ward was better than other wards, as there was often an option of a cooked breakfast. But sometimes meals would not arrive or they were just inedible. The nurses were always great when things went wrong, even going so far as to go to the hospital canteen to get me something. But bringing a good selection of snacks when being admitted is essential!
Eating with lymphoma
While all of the above make eating and maintaining weight a challenge. There is a lot that you can do and I was gradually able to put on weight later in the treatment.
Getting the calories
Despite an aversion to vegetables, I was used to eating generally very healthily, with plenty of fresh food and always maintaining a good weight. However, with the lymphoma, I needed to change my focus to eating the maximum calories I could. Unfortunately, this was a lot easier to do with less healthy preprocessed foods. My dietician explained this to me as “what is healthy for people is different, for you getting calories is more important than anything else right now”.
The kind of things I added to my diet were:
- High-calorie breakfast cereals (granola, honey-nut cornflakes etc)
- Fruit smoothies with oats
- A mid-morning sausage/egg sandwich
- Afternoon tea or snack
- Small starter an hour before dinner
- More desserts
- Milky drinks (hot chocolate, Horlicks etc).
Fatigue can make cooking meals difficult. If you have other people who can prepare dinner, great! If not, batch-cooking foods and freezing them on good days really helps on those days when you really don’t feel like cooking. Beef bourguignon, stews, lasagna, risotto, and curries all made good freezing for me. Family and friends often want to help and bringing around a home-cooked dish is a simple thing they can do to help. My mum’s “cancer casseroles” kept my fridge well stocked!
Snacks
Snacking regularly throughout the day is much easier than eating large meals. Peanuts, fruit, yoghurts, pork pies and cream cakes were some of my regular high-calorie snacks.
Supplements
At various points, I wasn’t able to get enough nutrition or calories from my diet alone. The hospital dietitian prescribed various things to help when this happened:
- Scandi-shakes: a medical milkshake that is very calorie dense and especially good when its difficult to take solid food
- Fortified drinks: not very pleasant tasting, but full of vitamins
- Multi-vitamin tablets.
These were put on repeat prescription for me at my GP, so I could get them whenever I needed them.
Other things that can help
Encouragement from other people
There were many days when I just didn’t feel like eating. My family and friends helped me by encouraging me to eat, even when I didn’t want to.
Weight scales
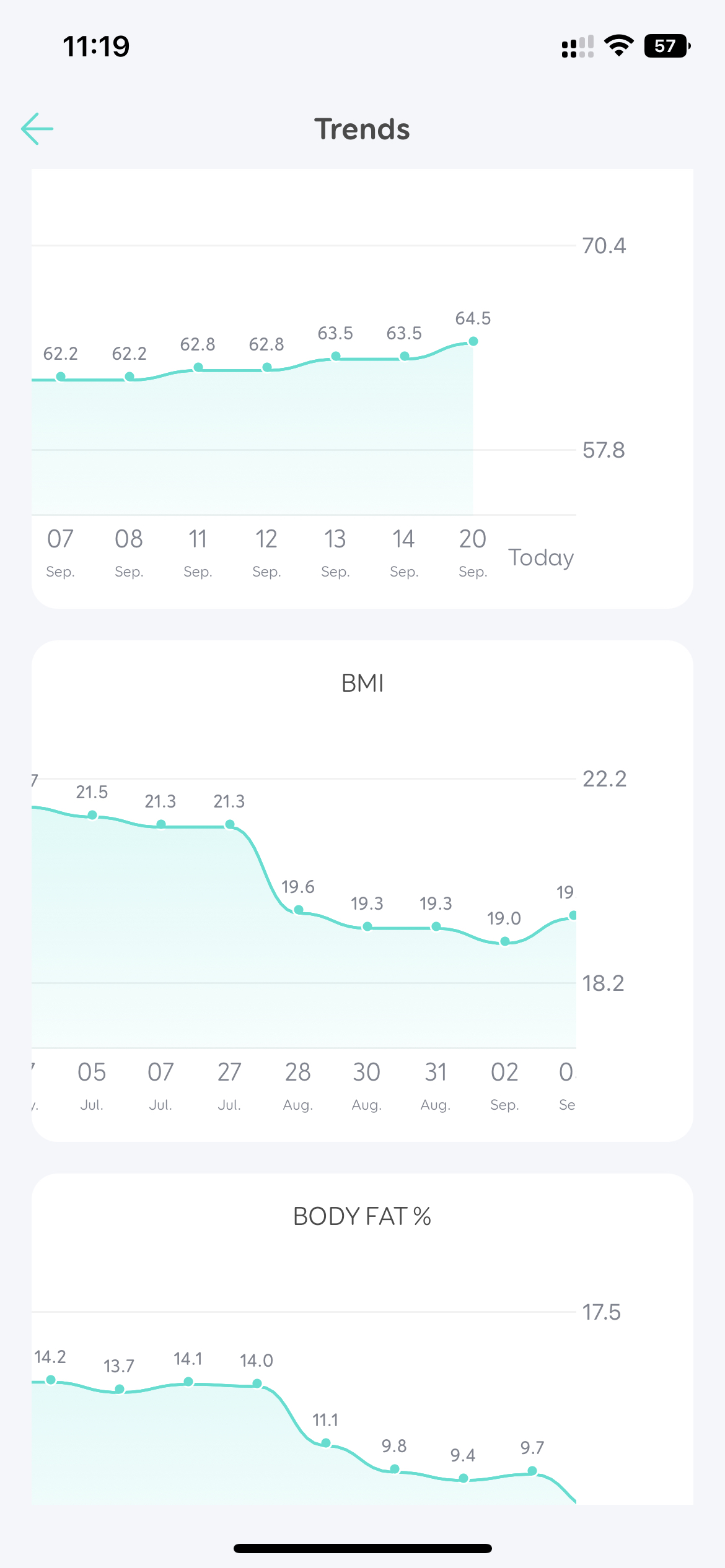 Having a set of good digital weight scales was essential to help me monitor my weight and encourage me to eat. I would weigh myself every morning and, using Bluetooth, my phone would keep a graph over time of just how I was doing.
Having a set of good digital weight scales was essential to help me monitor my weight and encourage me to eat. I would weigh myself every morning and, using Bluetooth, my phone would keep a graph over time of just how I was doing.
References
- 1
- 2
